por
John R. Fischer, Senior Reporter | March 07, 2023
A study found that an AI tool could identify abnormal chest X-rays with 99.1% accuracy.
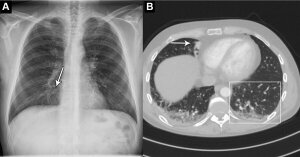
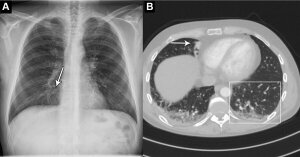
In a retrospective, multicenter study of 1,529 patients, researchers in Denmark identified abnormal chest X-rays with 99.1% sensitivity using Oxipit's deep-learning based solution, ChestLink version 2.6.
This was compared to 72.3% sensitivity among radiologists. Additionally, it had 6.3% higher sensitivity than the radiologists for detecting critical abnormal X-rays, at 99.8% compared to 93.5%.
If such accuracy could be found in larger prospective evaluations, the tool has the potential to alleviate heavy workloads faced by radiologists globally, they say.
"Radiologists are overworked, and the burnout rate is high across the globe. I don't think AI is the main solution for this problem, but if it can help in selected areas we should definitely test the possibility, because we need all the help we can get," co-author Dr. Louis Lind Plesner, from the department of radiology at the Herlev and Gentofte Hospital in Copenhagen, told HCB News.
Primary drivers of burnout rates include the global shortage of trained radiologists and the growing demand for medical imaging, especially cross-sectional such as CT and MR, says Plesner.
ChestLink is the only AI tool approved for autonomous usage (it is only approved in Europe at this time). The researchers applied it to chest X-rays from emergency department patients, in-hospital patients and outpatients at four hospitals in the capital region of Denmark. The solution classified scans as high-confidence normal (normal) or not high-confidence normal (abnormal).
Two board-certified thoracic radiologists evaluated each scan, and a third was used to break disagreements between the first two. All three were blinded to the AI results.
They classified 429 chest X-rays as normal. From this, the AI tool deemed 120 (28% of the 429) the same. These X-rays made up 7.8% of all X-rays and could be potentially safely automated by an AI tool, according to the researchers.
Plesner says ChestLink's high sensitivity for identifying all kinds of chest diseases was surprising, and that he and his colleagues could not find a single chest X-ray where the algorithm made a major mistake.
Further, he said it was especially useful among the outpatient group, identifying normal X-rays at a rate of 11.6%. Because of the high prevalence of normal chest X-rays in outpatient settings, the tool could prove to be a welcome addition by allowing radiologists to focus their time more on complex matters.
But he warns that while AI will become the standard of care someday, the solution in its current form is not a replacement for radiologists.
"We need way more advanced AI tools to be able to replace radiologists for chest radiography reading, especially when the image is abnormal," he said. "For example these systems need to be able to compare findings with previous imaging, correlate to patient history and age, and interpret chest X-ray findings more accurately, grade them in size/severity, make further imaging suggestions. This is not on the horizon yet to my knowledge."
The researchers say they will run ChestLink "in the shadows" for several months and double check all autonomously reported cases. They will also evaluate the cost benefit in terms of how many chest radiographs in any institution can actually be autonomously reported and is this number satisfactory.
The findings were published in
Radiology, a journal of the Radiological Society of North America.